Jenny Williams, beloved wife, mother, friend (and one hell of a cancer fighter) passed away on Tuesday evening, 11pm NZT. Her deterioration was quick – she was not ill more than 24 hours and, in essence, most of her decline was in the last six . It was vastly quicker than any of us had expected (including Jenny) but she knew she had to go.
Part of Mum’s campaign, in writing Get Out Gertrude, was to present an honest and truthful look at what inflammatory and metastatic breast cancer looks like, so in this post I’m going to be honest and truthful about what those last few hours were like. If this is something that you will struggle with (or perhaps don’t want to burst into tears at work), please stop reading after the quote. I’ll end this section with a laugh – on Monday Mum was telling me that in this blog post I shouldn’t say that she “lost” her battle with cancer – she says that she is finally going to win, and just perish from her battlefield injuries!
Life will break you. Nobody can protect you from that, and living alone won’t either, for solitude will also break you with its yearning. You have to love. You have to feel. It is the reason you are here on earth. You are here to risk your heart. You are here to be swallowed up. And when it happens that you are broken, or betrayed, or left, or hurt, or death brushes near, let yourself sit by an apple tree and listen to the apples falling all around you in heaps, wasting their sweetness. Tell yourself you tasted as many as you could.
– Louis Erdrich, The Painted Drum; via A Happy Adventure
Mum had the best last week ever – she was awarded a recognition of achievement in the Bachelor of Social Work course she was completing (an additional blog post coming on that later); she finally got to meet a close Twitter friend on Friday and had great South American food with Sis S and Niece S; we had a fabulous family lunch at Elliott Stables on Saturday, in which she was able to make solid inroads into both her meals, something a little rarer lately; she was able to see C off at the airport on Sunday morning and spent a lovely afternoon with friends at home on Sunday afternoon.
Mondays were the days that her and I (OD) spent together and we had a great day! We ended up running a lot of errands that day – she had said that one of the most annoying things about needing the wheelchair was that it required someone to actually take her out of the house. We went and spoke with her florist friends about her funeral flowers and what she would like and stayed for probably an hour and a half just chatting about everything. We went to the picture framers and on the way she was trying to direct me how to drive (I grew up in the town that she and my dad live in – so I knew where I was going) and we had a big laugh about it. At the picture framers, Mum was still healthy enough to walk in (10 metres) although she needed a stool to rest on when we were inside. Mum’s artistic side meant that we were there for at least a good twenty minutes – she wanted these framed photos for YD to be perfect. A part of me does wonder whether she had at least some sort of subconscious idea of what was to come.
We went to the lawyers and paid an invoice – once again, Mum still feeling like she could walk the 10 metres or so to the entry of the offices. Then it was off again to Mum’s favourite local cafe for lunch where she ordered wedges and a ginger beer; finishing the ginger beer and half the wedges which was again a great effort compared to some of her previous eating. We walked through Farmers and she pointed out a baby t-shirt that she liked, but of course we thought we had more time to look at things like that (one of my bucket list things with Mum was to shop for baby clothes together as she wasn’t going to be around when we do have kids) – you better believe that yesterday I went back and bought that cute little baby shirt for my as-of-yet non-existant baby!
We went to the post office, we went to find a frame for her cerficate, we went and saw her friends at Lotto and the Chemist (owned by the same company and Mum used to work in the Lotto section). Mum had great chats with her friends and then we came home and she saw even more friends while I cooked a roast chicken. Despite eating a big (for her) lunch, Mum also had quite a bit of dinner. She was tired, but at that point so was I. It had been a long day. R (my husband) and I left, Mum went to bed.
In the night, Mum woke up with diahorrea and it became clear that one of her haemerhoids had burst and was bleeding quite a lot. In hindsight, this was probably the sign that things were changing but she’s had bad nights before. She woke up a second time and Dad stayed at home from work until Mum woke up in the morning. She was lethargic but otherwise fine. MD came home from school practicum early and helped Mum dress herself, but again she had had bad nights before and found these things difficult before, so we didn’t think too much of it. Because of the bleeding, MD, Mum’s Sis M and Sis F took Mum to the doctors, where he examined her and provided her with a barrier cream and no other medication. Mum was still coherent and able to move herself when being examined.
In the afternoon, YD came around with her carer, L. They were still able to carry on a conversation but Mum was very tired. As YD left, she told Mum that she “was very lucky to have her sisters her at this time” – out of the mouths of babes, right? Mum’s friend T made an impromptu visit and again, whilst tired, Mum was still coherent when T left at 5 pm.
It all went downhill very quickly from that point. Mum started to become less coherent, not realising that she was lapsing in consciousness in between periods of lucidity. I was called and blasted home the 40 kms from my parent-teacher interviews. When I arrived, Mum’s breathing was troubled and she kept on telling us that she was very tired. We tried to get her pain medication in her but she was finding it increasingly difficult to swallow and we could not move her without hurting her to get her to bed. The decision was made to call the hospice and they sent out nurses to check her out. Mum was aware that this was happening – in her lucid moments she was saying that she didn’t know whether it was the right time to go to hospice, how she was getting confused about things so maybe she should go to hospice, that we could see what she was like and if we thought it was right, it was right.
Two hospice nurses arrived and they diagnosed her as having some sort of systemic shock. She was cold in her extremities and she was clammy and they told us to call an ambulance. As the ambulance staff loaded her onto a stretcher, the hospice nurses took Dad (OH), MD and I aside and said that it would be highly likely that this was it, and that she would pass away tonight. From all accounts in the ambulance, she was still completely herself in her lucid moments, correcting Dad/OH when he was getting her medical history wrong.
MD and I jumped into the car and headed for the hospital, getting R, MD’s friend B, Sis M and Sis F on route to the hospital via phone. When we arrived, it was a very short time before Mum was moved into a monitoring room in the ED and the doctors and nurses that were to be with us for the rest of the evening arrived. The doctor said that given her current medical history, there was no point in poking her and prodding her with unneccessary tests. Their goal was just to make her comfortable for as long as she had left.
At this point , Mum started complaining of a lot of pain and was curling up on her side. The nurses quickly organised a line for morphine into her abdomen and gave her half a syringe. Mum was significantly more comfortable after this and was able to ease out onto her back. She was surrounded by most of the family as Sis F waited for R to arrive. During this time she just kept on repeating herself to us – you have to look after each other, you have to keep loving each other, you have to keep caring for each other. We were assuring her that we would and telling her that she could rest and let go, that this was the end. She said to us “Okay, I’ve gotta go, bye” and those were her last coherent words. Sis F came in to let me know that R had arrived and I went to tell him how serious things had got. In the intervening term, the nurse had come in to give her a muscle relaxant as her breathing had got very gaspy. We walked back into the cubical, told Mum “R’s here” and she took a big sigh. While she lived for a short time after that point, I think that in essence, everything that was Jenny at that point left the room. So typical of Mum that she felt like she couldn’t go until everyone important was there and everyone had someone there to support them.
The end came smoothly, with everyone she wanted around her. The doctor came to confirm death and was so respectful to Mum, still telling her what he was going to do to check her vital signs. The bereavement care person came and took us through the process of what was going to happen from here on out. The majority of the family was escorted through to the bereavement care room and Dad/OH and I stayed in the room, waiting for the orderlies to come and collect her. We laid the bed down flat and tucked mum in, staying and talking about her and to her.
Once we’d been moved though to bereavement care, they took Mum to make her comfortable in the viewing room. When we walked in, I was so happy to see her laid out with the beautiful purple blanket that her uni friends had bought for her in Whangamata. She was so excited about that blanket; she told me about it the minute I walked in the door of A’s bach. We spent a lot of time with her in the room, sharing stories of times gone by, having tears and having laughs. Leaving her at the hospital when Dad/OH and I had to head home at 2 am is one of the hardest things we’ve ever had to do.
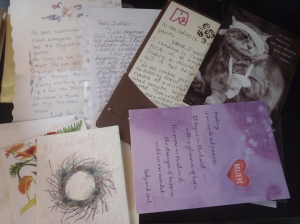
It’s been a whole day now since that happened – it seems surreal that she is gone. She had two blog posts that she really wanted to write and I’m going to do my best to write them on her behalf. Thank you so much for being the wonderful, supportive community that you have been – I know that we’ll never manage to thank all of you but you have all meant SO much, not only to Mum but to our whole family.